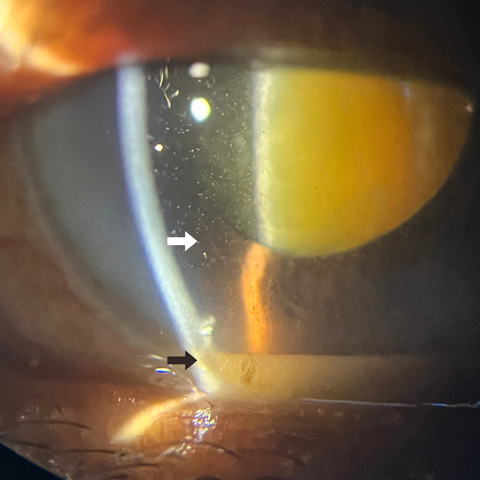
Glistening aqueous and pseudohypopyon—phacolysis without raised intraocular pressure
Main Article Content
Abstract
Phacolytic glaucoma is a rare secondary open-angle glaucoma. A 70-year-old woman presented at V N Desai Hospital, Mumbai, with gradual, progressive diminution of vision in her left eye of 6 months’ duration. Best-corrected visual acuity (BCVA) in the left eye was counting fingers close to the face. Slit-lamp examination of the left eye revealed minimal conjunctival congestion, clear cornea, and a deep anterior chamber with multiple refractile particles (white arrow) forming a pseudohypopyon (black arrow) and a hypermature (Morgagnian) cataract with an intact anterior lens capsule. Intraocular pressure (IOP) measured 14 mm Hg by Goldmann applanation tonometry. With lens aging, there is stretching of the anterior lens capsule. Degeneration of lens fibers of a hypermature cataract forms soluble, high-molecular-weight proteins that leak through microscopic openings of the intact lens capsule. These leaked proteins are phagocytosed by macrophages and can be seen as refractile particles in the anterior chamber, milky aqueous, pseudohypoyon, or white deposits on the anterior lens capsule. They can block the trabecular meshwork, resulting in raised IOP, which manifests as acute pain, redness of conjunctival hyperemia, and corneal edema. Cataract extraction is the definitive treatment for phacolytic glaucoma. Our patient had not developed raised IOP and had a clear cornea. She underwent successful small-incision cataract surgery in the left eye. Postoperative BCVA was 20/40. The classical pathophysiological findings in this case are not easily appreciated in more typical presentations with dense corneal edema due to elevated IOP.
Downloads
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.