Acute annular outer retinopathy
Main Article Content
Abstract
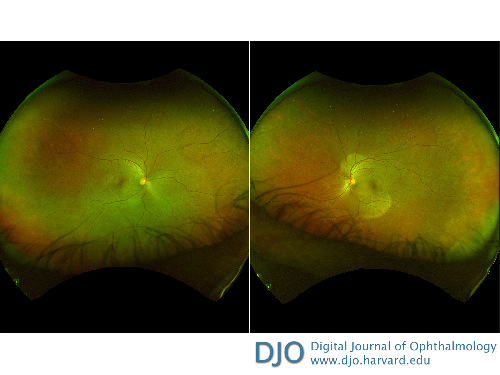
A 52-year-old man presented at the Veterans Affairs Hospital in Durham after 4 weeks of decreased vision in both eyes, bilateral central scotomas that lasted 2 weeks and improved, persistent flashing lights in both eyes, and increased bitemporal floaters. Visual acuity on presentation was 20/40 in the right eye, 20/60 in the left eye, decreased from 20/25 in the right eye and 20/20 in the left eye 2 months earlier. Dilated fundus examination was significant for a gray-white annular ring in both eyes, without vitreous cell. The patient was diagnosed with acute annular outer retinopathy. Review of systems was negative for infectious symptoms, and viral serology was negative for varicella zoster virus, cytomegalovirus, and herpes simplex virus. Epstein-Barr virus IgG was positive, suggesting a past infection. The risks and benefits of treatment with steroids was considered. Ultimately, the patient was not started on treatment, because he reported, via telephone, a subjective improvement in his vision 1 week after initial presentation. The patient returned to clinic 3 months after initial presentation, and visual acuity was 20/25 in both eyes.
Downloads
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.